Critical physiology: flow dynamics in intensive care

Flow dynamics and its application in critical care
Fluid dynamics has a wide range of applications in critical care, starting from high flow nasal cannula to high frequency ventilations, I am going to simplify the concept as i understood during my residency in pediatric intensive care
Lets start with some basic terminology
Fluid dynamics is a subdiscipline of fluid mechanics that study fluid flow.Dynamics is a science of fluids (liquids and gases) in motion.Rheology is the study of the flow of matter, primarily in the liquid state.
Terminologies: 4 basic terms
1. Velocity
2. Pressure
3. Density
4. Temperature
Types of flow: Lamellar vs Turbulence
An object moving through a gas or liquid experiences a force in direction opposite to its motion.
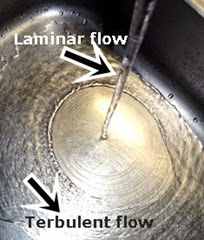
Image source: Google images
Laminar flow
occurs when a fluid flows in parallel layers, with no disruption between the layers. At low velocities the fluid tends to flow without lateral mixing, and adjacent layers slide past one another like playing cards.
There are no cross currents perpendicular to the direction of flow.
In laminar flow the motion of the particles of fluid is very orderly with all particles moving in straight lines parallel to the pipe walls (Parabolic velocity profile).
In fluid dynamics, laminar flow is a flow regime characterized by high momentum of diffusion and low momentum convection.
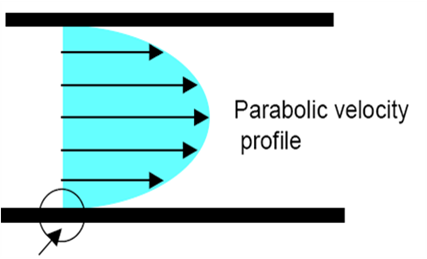
Image source:unknown
This flow profile of a fluid in a pipe shows that the fluid acts in layers and slides over one another.
Arrow shows adhesive forces between fluid and surface and relatively stationary flow at surface. Flow velocity increases towards the center gradually.
How to decide which type of flow ?:
Laminar and Turbulent flows is characterized and quantified by using Reynolds Number established by Osborne Reynolds and is given as

Where v = mean velocity, D = vessel diameter, ρ = blood density, and η = blood viscosity
If NR < 2000 – laminar flowNR > 4000 – Turbulent flow
Thus Higher velocity and lower viscosity favours the lamellar flow, The GOOD FLOW
Dont be surprise, we are intelligent cause Reynolds number for Blood flow in brain ~ 100 and Blood flow in aorta ~ 1000
Application:
1) AIRWAY OBSTRUCTION
Flow in the large airways is turbulent, and the resistance in thE flow is density dependent. In cases of extreme large-airway obstruction, the resistance can be reduced by reducing the density of the gas with the use of a mixture of helium and O2 (Heliox).
This reduction may help to relieve obstruction such that intubation of the patient is avoided. The primary limitation is the O2 requirement of the patient that dilutes the helium in the mixture.
2) HIGH FREQUENCY VENTILATION
From estimates of the Reynolds number and the dimensions of the airways obtained flow in the larger airways is turbulent. Laminar flow becomes established between the 4th and the 15th generation of airways, depending on the flow rate of the gas.
If the gas in a long, straight tube is moved in a laminar fashion by a sinusoidal pressure generator, the flow profile has to reverse with each cycle. The gas in the center of the tube will reverse velocity greater than that close to the wall. This type of flow movement is responsible for gas mixing in HFOV
3) VENTILATION
Airway resistance is also affected by the aerodynamics of flow through tubes. Flow through the airways is driven by a pressure drop between the alveoli and the endotracheal tube (Bernoulli's principle). In laminar flow, the gas has a precisely ordered velocity profile, and has the least possible pressure drop or energy dissipation for a given flow and tube diameter therefore unnecessary kinks in vent tubes as well as inappropriate tube diameter should be avoided.
It is also relevant in small endotracheal tubes for newborns during conventional ventilation of >60 breaths/min, when the inertia of the gas can cause an underestimation of airway pressure of several cm H2O.
4) CARDIOVASCULAR BLOOD FLOW
No turbulence occurs until the velocity of flow becomes high enough to break flow lamina. Therefore, as blood flow velocity increases in a blood vessel or across a heart valve. there is not a gradual increase in turbulence, Instead, turbulence occurs suddenly when a specific Reynolds number (Re) is reached.
Image source:cvsphysiology.com
In large arteries at branch points, in diseased and narrow arteries and across stenotic heart valves laminar flow can be disrupted and become turbulent. When this occurs, blood does not flow linearly and smoothly in adjacent layers, but instead in chaotic fashion, this can also occur in ascending aorta cause of high flow velocity.
Constriction of an artery also increases the velocity of blood flow through the constriction, producing turbulence and sound. Examples are bruits over constricted arteries and the Korotkoff sounds.
Turbulence occurs more frequently in anemia because of lower viscosity. This may be the explanation of the systolic murmurs that are common in anemia.
Elevated cardiac outputs, even across anatomically normal aortic valves, can cause physiological murmurs because of turbulence.
PERFUSION PRESSURE AND TUERBULENT FLOW

Image source:cvsphysiology.com
Turbulence increases the energy required to drive blood flow by increasing the loss of energy in the form of friction, which also generates heat.
When plotting a pressure-flow relationship (see figure above), turbulence increases the perfusion pressure required to drive a given flow. Alternatively, saying at a given perfusion pressure, turbulence leads to a decrease in flow.
NEWTONIAN AND NON-NEWTONIAN FLUID
Newtonian fluid obeys the law that viscosity of fluid remains constant regardless of any external stress that is placed upon it, at constant temperature and pressure.
For, Non-newtonian fluids, flow is affected by their viscosity and affected differently for different fluid due to different coefficient of viscosity (n).
What generates Viscosity ?
When fluids flow they have a certain amount of internal friction called viscosity. It exists in both liquids and gases.
Whats is coefficient of viscosity?
Fluid in contact with surface is held to that surface by adhesive forces between the molecules of the fluid and surface. Therefore, the molecules at the surface of the stationary wall are at rest and the molecules at the surface of the moving plate will be moving with velocity v.
The layer of fluid in contact with the stationary wall will retard the flow of the layer just near to it. This layer will retard the layer near and so on. The max flow velocity will be present in centre. With different adhesive forces for different fluid, the velocity will vary. This is coefficient of viscosity (n).
Different fluid have different coefficient of viscosity. It is one of the several determinants of flow rate of gases and blood in body.
Earlier, blood was treated as a Newtonian fluid. However Thurston reported that The viscoelastic properties which make human blood non- Newtonian depend on the elastic behavior of red blood cells.
“Blood is not a Newtonian fluid. (Viscosity differs constantly). The viscosity depends strongly on the fraction of volume occupied by red cells (Hematocrit).”
Viscosity of blood increases with
- Increased hematocrit
- Constrictions in vessels
- Decrease flow rate of blood through vessel (RBCs adhere to each other, and the vessel walls.)
Viscosity of blood decreases with
- Increased flow velocity
- Vessel diameter below 300 μm (Reduced η when RBCs get aligned in small vessels. (This is called as Fahraeus-Lindqvist effect.)
- In very small vessels (< 20 μm), η increases as RBCs fill the capillaries, “tractor tread” motion.
DYNAMICS OF BLOOD FLOW (RHEOLOGY)
The macroscopic rheologic properties of blood are determined by its constituents.
In large arteries, the shear stress exerted on blood elements is linear and blood behaves as a newtonian fluid. In the smaller arteries, the shear stress acting on blood elements is not linear and therefore it become non-newtonia
APPLIED PHYSIOLOGY
The aorta and arteries have a low resistance to blood flow compared with the arterioles and capillaries.
When the ventricle contracts, a volume of blood is rapidly ejected into the arterial vessels. Since the outflow to the arteriole is relatively slow because of their high resistance to flow, the arteries are inflated to accommodate the extra blood volume. During diastole, the elastic recoil of the arteries forces the blood forward into the arterioles.
Thus, the elastic properties of the arteries help to convert the pulsatile flow of blood from the heart into a more continuous flow through the rest of the circulation.
The Moens-Kortweg wave speed
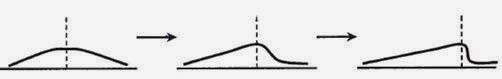
(Steeping of pressure pulse with increasing distance away from heart)
Concept was obtained by Thomas Young in 1808, and is known as the Moens-Kortweg wave speed. Steepening of the pressure front as it travels from the heart toward the peripheral circulation . Wave speed also varies with age because of the decrease in the elasticity of arteries and increasing intramural pressure.
INVASIVE BP WAVEFORM
The arteries are not infinitely long, and it is possible for the wave to reflect from the distal end and can travel back up the artery to add to the pressure.
In patient with high blood pressure there can be increase reading in systolic BP than actual BP called as pressure augmentation due to above effect
FLOW IN CURVED TUBES
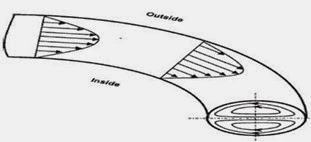
The arteries and veins are generally not straight but have some curvature, especially the aorta, which has a complex three-dimensional curved geometry.
Effect of curvature on blood flow, can be understood by a steady laminar flow in a plane curved tube .
When a steady fluid flow enters a curved pipe in the horizontal plane, all of its elements are subjected to a centripetal acceleration relative to their original directions and directed toward the bend center. (SEE ABOVE IMAGE)
Branching is clearly an important contributor to the measured pressures in the major arteries. (HIGH)
FLOW IN MICROCIRCULATION
Concept of a closed circuit for the circulation was established by Harvey (1578–1657). The experiments of Hagen (1839) and Poiseuille (1840) were performed in an attempt to explain the flow resistance of the human microcirculation.
The term “microcirculation” is for vessels with internal diameter that is multiple of major diameter of the RBC. This definition includes primarily the arterioles, the capillaries, and the postcapillary venules.
The capillaries are of particular interest because they are generally from 6 to 10 μm in diameter, which is about the same size as the RBC. In the larger vessels, RBC may tumble and interact with one another and start moving streamlined as they travel down the vessel. In contrast, in the microcirculation the RBC must travel in single file through true capillaries.
Therefore,
The viscosity of blood has a primary influence on flow in the larger arteries, while the elasticity, which resides in the elastic deformability of red blood cells, has primary influence in the arterioles and the capillaries.
If you like this post, or suggest any additions comment below, share too ! See you for the next post
References:
1. Ganongs Review of medical physiology
2. Wikipedia for images
3. Fluid flow, viscosity, poiseuille's law. visual physics. school of physics university of SydneyAustralia.
💡 Join the Discussion!
🩺 Help us refine this article — share corrections or additional information below. Let's elevate the accuracy of knowledge together! 💉💬